What You Need To Know About Stretching
Lindsay Wilde, SPT and Chris Mooney, DPT • March 26, 2020
Chances are, at some point in your life you have been told that you need to stretch more. But is stretching actually worth it? The claimed benefits of stretching are that it increases flexibility, improves performance, and decreases the risk of injury. However, recent research on stretching is varied and controversial. Because of the discrepancies in the research, it’s logical to question if stretching is actually worth it.
Overview and Background Information: Range of Motion (ROM)
is defined as the degree of movement that occurs at a joint. Flexibility
is a measure of that range of motion and it has both a static and dynamic component to it. Static flexibility
is the range of movement at a joint and its surrounding musculature that occurs with passive movement. Static flexibility does not involve any voluntary muscle activity and is done using gravity, a partner, or a machine. Dynamic flexibility
is the available range during active movement and requires voluntary muscle action. Although a certain degree of motion about a joint is considered “normal”, the relationship between flexibility and performance is questionable. Therefore, it’s important to understand that normal range of motion does not necessarily guarantee normal movement. Other factors such as muscle strength and motor control are needed for normal movement. Another key concept to understand is that the amount of range of motion an individual requires depends on the demands they place on their body. For example, a gymnast or a dancer require more flexibility than a powerlifter or football player. Therefore, it is important to keep in mind that the flexibility demands for each person may vary.
Types of Stretching: Static Stretching:
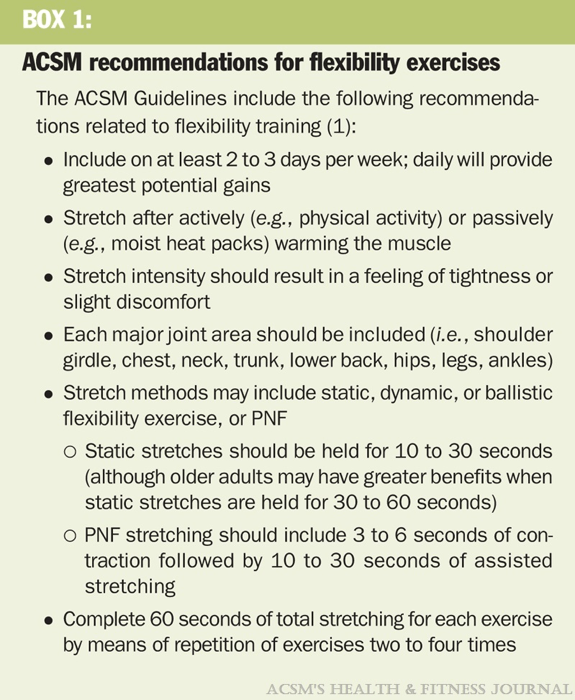
Defined by the American College of Sports Medicine (ACSM) as a technique that involves a slow and constant stretch at end range or point of mild discomfort that is typically held for 15-30 seconds. This type of stretch is considered static because it is held at end range for a period of time, without any additional movement. Because static stretching is done in a controlled manner it is considered appropriate for all individuals for increasing flexibility.
Ballistic Stretching: Ballistic stretching is defined as stretching that involves active muscular effort and uses a bouncing-type movement. The ASCM no longer recommends this type of stretching for increasing range of motion and flexibility, even though ballistic stretching just as effective as static stretching at increasing range of motion. This is due to the high-intensity nature this type of stretching and the degree of muscle tension that occurs during ballistic stretching puts the individual at an increased risk for injury thus making it inappropriate for some individuals. Ballistic stretching is also more likely to stimulate receptors within the tissue that lead to muscle guarding and therefore full range of motion may actually be limited.
Dynamic Stretching: Dynamic stretching is similar to ballistic stretching, in that it involves active muscle contraction, however unlike ballistic stretching, it avoids bouncing and is performed in a more controlled manner. Dynamic stretching is not only more controlled but it also uses sport-specific movements to help prepare the body for activity. Dynamic stretching is designed to increase core temperature, enhance activity-related flexibility and balance, and prepare the body for performance. This type of stretching is typically done prior to exercise, whereas static stretching is done post-exercise.
Proprioceptive Neuromuscular Facilitation (PNF) Stretching: Originally developed for patients with muscle tone issues due to neurological conditions, PNF stretching helps to facilitate muscle relaxation. PNF stretching is typically performed with a partner and combines both active and passive muscle actions. There are three types of PNF stretching, all of which include a passive stretch and an active muscle contraction, which is then followed by a passive stretch. The three types of PNF are hold-relax, contract-relax, and hold-relax with agonist contraction. Some studies have concluded that PNF stretching is superior to static stretching and ballistic stretching at improving range of motion, but the research is varied and controversial.
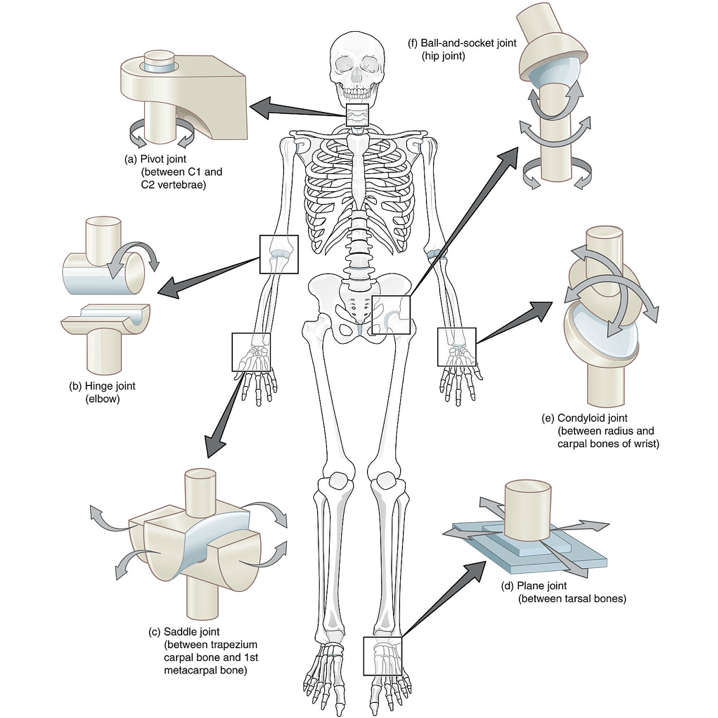
Factors Affecting FlexibilityJoint Structure: The structure of a given joint determines the amount of available motion at that particular joint. Ball-and-socket joints (hip and shoulder) have the greatest degree of available motion and are able to move in all planes of motion. Therefore, these types of joints are expected to have a larger degree of motion than hinge joints (elbow and knee).
Age and Gender: As we age, a process called fibrosis takes place throughout our body, in which fibrous connective tissue replaces degenerating muscle fibers. This fibrous connective tissue is not as elastic as the muscle fibers it replaces and therefore the pliability of the tissue decreases along with the available range of motion. Gender also plays an important role in flexibility, due to the anatomical and hormonal differences between females and males. Anatomical differences in pelvic shape and size between males and females, along with increased estrogen and progesterone production in females account for increased flexibility in females when compared to their male counterparts.
Muscle and Connective Tissue: Elasticity is the ability to return to original resting length after passive stretch, while plasticity is the ability to assume a new and greater length after passive stretch. Both the elasticity and the plasticity of the tissue affect the flexibility and the available range of motion. There is a variety of different tissue types throughout the body (muscle, tendon, ligament, fascia, etc.) and each type has its own degree of elasticity and plasticity. Therefore, the characteristics of the surrounding tissue will determine the available range of motion.
Activity Level: Active individuals tend to be more flexible than inactive individuals. This is particularly true if the individual performs activities that require a high degree of flexibility (yoga, gymnastics, etc.) Although active individuals tend to have a greater degree of flexibility, activity level along does not improve flexibility. A comprehensive training and stretching program is needed in order to positively affect range of motion and overall flexibility. It is also important to exercise and move a joint throughout its full range of motion. In doing this not only is flexibility maintained but the surrounding muscles are strengthening at all ranges of motion but joint health is also facilitated.
Stretch Tolerance: Stretch tolerance is the ability of an individual to tolerate the discomfort of a stretch. Those with a greater stretch tolerance tend to have a greater degree of flexibility and therefore greater range of motion. The discomfort from stretching comes from stimulation of receptors within the tissue. These receptors help to sense the amount of stretch and tension that is occurring in the tissue and activation of these receptors can lead to discomfort during stretching as well as increased muscle guarding and tension.
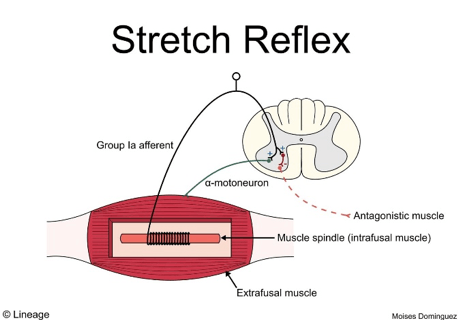
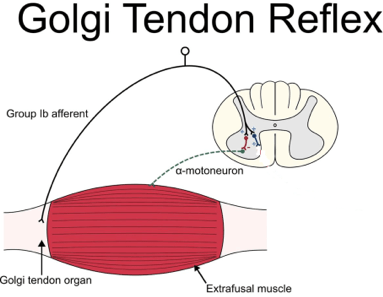
Muscle Spindles & Golgi Tendon Organs (GTO)
With the muscle, there are two important receptors that determine muscle length and muscle tension and therefore can affect flexibility and the available range of motion during stretching. Muscle spindles are located within the muscle fiber and sense changes in the muscle length. If the muscle is rapidly stretched, the muscle spindle is activated and causes the muscle to contract and shorten in length, therefore limiting the degree of motion. However, if the stretch is performed in a slow and gradual manner, the muscle spindle is not activated and the muscle is able to lengthen to its full extent. Because of the slow movement that occurs in static stretching and PNF stretching, these stretching techniques are typically favored when it comes to increasing flexibility and range of motion, while dynamic and ballistic stretching are not. The Golgi tendon organ (GTO) is another receptor that is located at the musculotendinous junction (where the muscle merges into the tendon). The GTO is sensitive to the amount of muscle tension within the muscle. When muscle tension reaches a certain level of intensity, the GTO is stimulated and results in muscle relaxation and therefore a reduction in the amount of tension developing within the muscle. Manipulation of the GTO can be beneficial when it comes to trying to improve the flexibility of a muscle, because a relaxed muscle with have greater motion than a muscle that is guarding or has increased tension.
When, How Much, and How Long?
So if you do stretch, how long and how often should you be stretching? Just as the types and benefits of stretching are controversial, so is the duration and frequency of stretching. According to the American College of Sports Medicine and the National Strength and Conditioning Association (NSCA), static stretching should be held for anywhere between 15-30 seconds, although some sources say as low as 10 seconds is sufficient, and that the stretch should be repeated no more than 4 times (because there were only minimal gains with additional repetitions). When an individual should stretch depends on the type of stretching being performed. The NSCA states that stretching with the goal of improving ROM and flexibility should be done following activity (within 5-10 minutes after activity) and as a separate session. When stretching is done as its own session, it should be proceeded by a general warmup in order to allow an increase in muscle temperature which is necessary for effective stretching. While most sources advocate 15-30 second hold for static stretching, recent research has explored the effectiveness of different durations of stretching along with total stretching time. While the research regarding the effectiveness of different durations of stretching is controversial, what is consistent is that at least 4 repetitions of a particular stretch should be performed and any additional repetitions performed after 4 resulted in only minimal improvement. The biggest limitation with a lot of the research on stretch frequency and duration is the limited subject pool. The majority of the stretching research has been conducted using healthy individuals under the age of 40 meanwhile, those individuals who may benefit the most from stretching (ex. elderly and post-surgical patients) are excluded. According to an article that look at stretching in the elderly population (>65 years old), holding a stretch for 60 seconds was more effective at increasing ROM than holding the stretch for only 15 or 30 seconds. Although, stretching for all three durations lead to increases in ROM, holding the stretch for 60 seconds lead to a faster rate of ROM improvement compared to the 15 second and 30-second stretch. Older individuals and the elderly may benefit from longer durations of stretching, due to the effect that aging has on flexibility and the fibrotic changes that occur throughout the body with increasing age.
So Is It Worth It?
Although some stretching techniques have been found to be more effective than others and there are inconsistencies in the research. However, stretching can help to improve flexibility and range of motion and therefore is an important factor when it comes to overall musculoskeletal health. Static stretching is considered the safest and everyone is able to safely perform static stretching so along a proper technique is used. Although 4 repetitions held for 15-30 seconds is the accepted dosage for static stretching, the evidence regarding the value of holding a stretch for 15 seconds versus 30 or 60 seconds is controversial and continues to be a topic of debate. Due to the effect aging has on flexibility, holding a stretch for longer durations (60 seconds) may be more beneficial in older or elderly populations. Although most individuals would benefit from incorporating a stretching routine into their daily lives, there are times when stretching may be contraindicated. In individuals who have Ehlers-Danlos Syndrome or Marfan Syndrome, aggressive stretching is contraindicated because these individuals are hypermobile and therefore have an increased amount of available motion to being with. Therefore, stretching for these individuals can actually lead to excessive motion and instability at the joints. The primary concept to understand is that each individual’s needs are specific and unique. Although most individuals would benefit from general stretching and flexibility exercises, individuals suffering from injury or pain may have specific needs that may not be addressed with a generalized program and require input from a trained strength and conditioning coach or physical therapist.
If you or anyone you know has questions regarding stretching or how it may benefit you please call us at 410-628-0520.
References:
1. American Heart Association. (2020). Flexibility Exercise (Stretching). [online] Available at: https://www.heart.org/en/healthy-living/fitness/fitness-basics/flexibility-exercise-stretching [Accessed 19 Feb. 2020].
2. Bandy, W. and Irion, J. (1994). The Effect of Time on Static Stretch on the Flexibility of the Hamstring Muscles. Physical Therapy, 74(9), pp.845-850.
3. Feland, J., Myrer, J., Schulthies, S., Fellingham, G. and Measom, G. (2001). The Effect of Duration of Stretching of the Hamstring Muscle Group for Increasing Range of Motion in People Aged 65 Years or Older. Physical Therapy, 81(5), pp.1110-1117.
4. Haff, G. and Triplett, N. (2016). Essentials of strength training and conditioning. 4th ed. Champaign, IL: Human Kinetics, pp.317-328.
5. Hoffman, J. (2012). NSCA's guide to program design. Champaign, Ill.: Human Kinetics, pp.51-70.
6. Magyari, P., Lite, R., Kilpatrick, M. and Schoffstall, J. (2018). ACSM's Resources for the Exercise Physiologist. 2nd ed. Philadelphia: Wolters Kluwer, pp.121-127.
7. Mayo Clinic. (2020). Stretching is not a warm up! Find out why. [online] Available at: https://www.mayoclinic.org/healthy-lifestyle/fitness/in-depth/stretching/art-20047931 [Accessed 19 Feb. 2020].
8. Page, P. (2012). Current Concepts in Muscle Stretching for Exercise and Rehabilitation. The International Journal of Sports Physical Therapy, 7(1), pp.109-119.

Running is one of the most common and popular methods of fitness in the world, with many cities and communities taking part in establishment of running events from 5k to marathon level and above, to smaller running cohorts, and for social events. However, while running has a high link to overall improved cardiovascular wellbeing, it is also one of the most injury prone athletic populations in world with injury incidence of up to 80%! Fortunately, there are many strategies to help combat and prevent running related injuries for any skill level. TRAIN APPROPRIATELY! As with any other sport, training for the specific demands of running can greatly reduce the risk of injury. The World Health Organization (WHO) recommends a minimum of 150 minutes of moderate-intensity aerobic physical activity or 75 minutes of vigorous-intensity physical activity throughout the week, based on strong evidence of health benefits and reductions upon mortality rates. While many factors influence risk of injury, there are a few significant ones for any running athlete: Type of exercise Find the aerobic exercise that you are passionate about! However, limiting yourself to the same route and same type of run could increase your risk for injury. Cross training with other modes of exercise including strength training or different types of runs could help reduce risk of chronic and acute injury! Exercise frequency and progression Novice runners may benefit from having more days of recovery, especially in the beginning. However, knowing when to progress overall speed, distance, or number of training days can be tricky! Remembering to increase only one variable at a time can help mitigate risk of injury. Exercise intensity and duration Having trouble with determining how intense your run is? Heart rate is an excellent measure of overall cardiovascular output. An easy calculation for determining your Heart Rate maximum is: 220-age As stated prior, recommended minimums for health benefits are 150-300 minutes of moderate intensity, or 75-150 minutes of vigorous intensity per week that typically are broken up into 3-5 days during the week. However, do not let these recommendations deter you from running if you cannot reach them! Calculate using % of Maximum Heart rate, Moderate intensity for aerobic exercise 60-75% of your calculated Heart Rate max; vigorous intensity 75-90% of maximum Heart Rate Equipment Matters! In a recent systematic review of 15 studies there was moderate to strong evidence of higher injury prevalence with persons who had sustained a previous injury, as well as the use of orthotics and the same pair of running shoes for longer than 4-6 months. While there are many different brands and trends within the running shoe and orthotic industry, it is important to note that finding the right pair of shoes for you may take time! Additionally, according to a study on use of multiple shoes during training, results found that there was a 39% decrease in running related injuries over a 22-week period when athletes used at least one more pair of running shoes during the week. Rehab potential 80% of all running injuries are result of overuse or chronic pathology, which may be a result from overtraining or limited tissue adaptations from the amount of load produced on the body during activity. Different types or locations of injury require methods of individualized rehabilitation, and the therapy experts at Evolution Sports Physiotherapy are well versed in the appropriate rehabilitation and progression of any running related injuries. So, whether you are a seasoned runner looking for a full evaluation of running form, or a beginner working towards your first 5K, our approach towards integration of best available evidence within clinical practice and dedication to patient care provides our patients with optimal rehabilitation potential. If you or anyone you know has suffered a running related injury, please contact us via phone at 410-628-0520 or email at chris.mooney@evolutionsportspt.com. We look forward to answering any of your questions and assisting with all of your rehab needs! References 1. Kozlovskaia M, Vlahovich N, Rathbone E, Manzanero S, Keogh J, Hughes DC. A profile of health, lifestyle and training habits of 4720 Australian recreational runners-The case for promoting running for health benefits. Health Promot J Austr. 2019 Apr;30(2):172-179. 2. van der Worp MP, ten Haaf DS, van Cingel R, de Wijer A, Nijhuis-van der Sanden MW, Staal JB. Injuries in runners; a systematic review on risk factors and sex differences. PLoS One. 2015;10(2):e0114937. Published 2015 Feb 23 3. Francis P, Whatman C, Sheerin K, Hume P, Johnson MI. The Proportion of Lower Limb Running Injuries by Gender, Anatomical Location and Specific Pathology: A Systematic Review. J Sports Sci Med. 2019;18(1):21-31. Published 2019 Feb 11 4. Malisoux L, Ramesh J, Mann R, Seil R, Urhausen A, Theisen D. Can parallel use of different running shoes decrease running-related injury risk?. Scand J Med Sci Sports. 2015;25(1):110-115.

Musculoskeletal Diagnostic Ultrasound (DU) is a powerful tool that can be utilized by Physical Therapists to identify tendonopathies. Furthermore, DU can be utilized with Dry Needling in order to visualize the needle which has been shown to significanlty improve the accuracy of the user to target the affected area compared to relying solely on palpation and anatomical landmarks.

The first installment in our running mechanics series discussed the importance of stability and striking your support leg under your hips. This Pose position will allow the runner to absorb forces more readily and prepare more efficiently for the next movement. The next movement in the Pose Method is the Fall. The purpose of this phase is to increase speed and since the Pose Method is all about “effortless running,” optimal body alignment will allow gravity to do the brunt force of the work.
The Pose Method of running allows one to identify and promote a running form that maximizes gravity along with the body’s effort and stored energy (elasticity) to create efficient movement. In essence, it makes running easier and less physically stressful to the body. There is a lot of debate surrounding running form. Some even question if it’s necessary to promote a particular way of running. However, it is a universally accepted foundation that every activity has a “best practice” - from changing a tire to playing basketball to cooking. As able-bodied individuals, we are all physically capable of performing such activities, but how long it will take to complete? How many unnecessary steps do we take? How much additional effort and load do we put on our bodies mentally and physically? These questions can be addressed by learning and PRACTICING ideal mechanics. Sure, you can go out on a 1-mile run in a recommended shoe to begin your fitness journey but would you start your golf journey on the tee box of Hole 1 with your newly purchased clubs? No, likely you would work with a knowledgeable person on how to hold the club, general swing mechanics and practice several range balls before venturing to the course. Why should running be any different? Particularly in a sport where “novice” runners have a much higher risk of running related injuries (RRI) compared to experienced runners. In a study completed in 2018, authors found a 2x-injury rate in novice runners compared to experienced runners over a 4-yr period. Secondly, running is the cornerstone of several other sports so as you go out to shoot 100 free throws every day to practice your form, why wouldn’t you add drills to improve the form of getting from Point A to Point B on the court? It makes sense to make use of the studies on running form and body mechanics to begin a new fitness goal in order to give us an advantage - how many YouTube videos do you watch before endeavoring to fix the washing machine? Knowledge is power. The Pose Method works by identifying repetitive “poses” during a running cycle through which every runner must pass: they have been described as Pose (the typical running “picture”), Pull and Fall. For the next few weeks, we will be breaking down each phase. We will start with “the Pose.”

In our previous blog post, we highlighted the peripheral mechanisms of dry needling into muscle tissue. The benefits of trigger point dry needling have been well documented in the literature. However, this is only one component of needling in the treatment of neuro-muscular dysfunction. A comprehensive definition of dry needling should include nerves, ligaments, tendons, scar tissue, bone and teno-osseus junctions.1 This requires expanding beyond the trigger point model to consider additional peripheral, spinal and supraspinal mechanisms. The classic local twitch response is thought to be a strong neural impulse triggered from needling into multiple sensitize loci. Mirror local twitch responses have been recorded in the opposite trapezius muscle during dry needling of the symptomatic trapezius. This example suggests a consideration of central mechanisms in addition to local muscle dysfunction.1 A brief review of pain physiology is helpful in consideration of central dry needling mechanisms. Pain sensation originates in peripheral nociceptors that continue into sensory fibers, which feed into the central nervous system through the dorsal horn of the spinal cord.2 After connecting with spinal neurons, the pathway continues up the spinothalamic and spinoreticulothalamic tracts. These lead to supraspinal locations including the thalamus, parabrachial nucleus and amygdala. There is significant potential for both dysfunction and pain relief within this neural system.2 Throughout this discussion, the terms acupuncture and dry needling will be used interchangeably.1 While many studies use the term “dry needling,” others commonly use terms including TrP acupuncture, acupuncture needling and electroacupuncture. Several studies have used acupuncture and dry needling in the same title. All of these cases meet the strict definition of “dry needling”. This trend of discussing dry needling as acupuncture is commonly seen in the UK, Canada, USA and Germany.1 Acupuncture randomized control trials and other studies have commonly used western medical diagnoses including neck pain, knee osteoarthritis and plantar fasciitis.1 Furthermore, these studies applied needles into “Ah-Shi points,” which is Chinese for “auwh that’s where it hurts” or “that’s it.” These are synonymous with trigger points and are used in combination with non-trigger point targets. In this sense, it is beneficial for physical therapists to recognize the findings of appropriate biomedical acupuncture research.1 Studies have demonstrated that electroacupuncture involves many different mechanisms and bioactive substances, both peripherally and centrally for pain conditions.3 Peripheral release of endogenous opioids originate from lymphocytes, monocytes/macrophages and granulocytes. Sympathetic nerve fibers are additionally activated for opioid response. These opioids activate receptors on peripheral nerve terminals to decrease pain signaling back to spinal and supraspinal structures.3 Electroacupuncture has been shown to inhibit the sensory component of pain through spinal mechanisms including opioids, serotonin, norephinephrine and glutamate.3 Spinal opioid receptors are targeted to inhibit thermal hyperalgesia and mechanical pain thresholds. Low and high frequency electroacupuncture have been found to inhibit thermal pain during acute pain. Thermal, mechanical and spontaneous pain are inhibited in persistent pain conditions. Electroacupuncture influence on opioid receptors is thought to occur on both presynaptic primary afferent fibers and postsynaptic dorsal horn neurons.3 Electroacupuncture studies have also confirmed the involvement of spinal serotonin and norephinephrine in pain inhibition.3 This includes serotonin-containing nucleus raphe magnus neurons and norepinephrine-containing locus coeruleus neurons. Electroacupuncture also decreases glutamate receptor activity and induces release of spinal norepinephrine, which each inhibit pain signals at the spinal level. Pain reduction has also been noted with changes in glial cells, cytokines, signal molecules/pathways, dopamine and acetylcholine at the spinal level.3 Electroacupuncture benefits via supraspinal mechanisms have been noted with the contribution of many nuclei.3 Sensory components are mediated via nucleus raphe magnus, periaqueductal gray, locus coeruleus, arcuate, preoptic area, nucleus submedius, habenular, accumbens, caudate, septal area and amygdala. Opioid activity in the arcuate-periaqueductal gray-nucleus raphe magnus-spinal dorsal horn pathway are thought to be particularly important in this sensory realm. Several studies have shown that endorphin release blocks affective pain responses while controlling for sensory pain inhibition. This selective supraspinal influence on affective and sensory components of pain is a similar consideration for drug efficacy in pain management, including the use of morphine.3 The physical therapists at Evolution Sports Physiotherapy have been trained in a variety of needling techniques to meet the individual needs of our patients. Our comprehensive treatment approach respects localized tissue dysfunction in addition to central considerations based on clinical findings and assessment. Please contact us with any questions concerning dry needling and treatment options. References: 1. Dunning J et al. Dry needling: a literature review with implications for clinical practice guidelines. Physical Therapy Reviews 19(4):252-265, 2014 2. Cagnie B et al. Physiologic effects of dry needling. Curr Pain Headache Rep. 17:348, 2013. 3. Zhang R et al. Mechanisms of acupuncture- electroacupuncture on persistent pain. Anesthesiology. 120:482-503, 2014.

This is probably the most common question asked by patients when dry needling is presented to them as a viable treatment option. The answer to this question is multifaceted. In this post, I will review the peripheral indications and effects of dry needling and will break down and discuss multiple attributes of the treatment. Dry needling is much more than simply inserting an acupuncture needle into a painful trigger point, tight muscular knot, or muscle spasm. Before we understand how the needle itself effects healing and pain levels, it is important to understand the body’s mechanisms that allow these conditions to form in the first place. Trigger points, or knots, can form for a variety of reasons to include acute trauma, repetitive micro-trauma, overuse, and stress. All of these conditions elicit an inflammatory healing response from the body, which creates compression of local blood vessels and decreases circulation and oxygen delivery to the area. This impaired circulation combined with the increased metabolic demands of the hypertonic muscle leads to the depletion of Adenosine Triphosphate (ATP), the cells energy source used to fuel metabolic processes. The “energy crisis” created via the decrease in available ATP creates compensations at the neuromuscular end plate, both pre- and post-synaptically . Pre-synaptically, in the nerve terminal, ATP is directly responsible for the inhibition of acetylcholine (ACh) release. Acetylcholine is a neurotransmitter used at the motor end plate to elicit a muscle’s action potential and therefore a muscle contraction. The depletion of ATP perpetuates the release of ACh, thus perpetuating a muscle contraction in an already hypertonic muscle. Post-synaptically, ATP fuels the calcium (Ca2+) pump, which is responsible for maintaining the electrochemical gradient required to signal skeletal muscle cells to contract. The calcium pump is utilized by opening to allow a stimulus signal to pass and thus allow Ca2+ to flood they cytosol, but also to immediately pump ca2+ out of the cytosol when muscle activation is no longer required. The depletion of ATP mentioned above allows these channels to remain open, therefore, the muscles continually receive the signal to contract. Both of these actions compound upon one another to create a vicious cycle of muscle hypertonicity. When the increased metabolic demands of the hypertonic muscle cell are not met, the cells begin to panic and essentially yell for help. This is achieved by releasing algogenic chemicals such as bradykinins, cytokines, serotonin, histamine, potassium, prostaglandins, leukotrienes, somatostatins, and substance P in order to activiate local nocicepors, to elicit a healing response from the body. Thus, we have the development of a trigger point and the subsequent tenderness and pain associated with it. The effects of prolonged exposure to algogenic substances have been shown to lead to demyelination of local nerves and abnormal nociceptive impulses, which perpetuate the pain cycle. One of the key components of the dry needling treatment is often the aim of eliciting a “twitch response” by inserting the needle directly into a trigger point and tapping onto a sensitive loci. Although this effect is not required for a successful dry needling treatment it is a key component in clearing the excessive build up of ACh from the synaptic cleft and returning the motor end plate to a homeostatic state. Needle manipulation also plays a key role in the effects of dry needling. Multiple techniques are used to achieve a variety of goals. The techniques of pistoning or fanning of the needle are often utilized to create microtrauma and to elicit twitch responses by tapping onto multiple sensitive loci in the desired area. Periosteal pecking is a technique often used at the teno-osseous junction to achieve small amounts of bleeding and microtrauma to a tendon that normally has very little blood supply, in order to elicit a healing response. This technique is performed by a series of rapid tapping motions through the tendon and onto a bony backdrop. Lastly, the needle manipulation technique of twisting the needle has been shown to have numerous effects on local tissues as well as pain relieving properties. Of all of the techniques discussed, only rotation of the needle has been shown to definitively change the appearance of the local connective tissue surrounding the insertion point. Marked thickening of the subcutaneous connective tissue along with deformation of the extracellular matrix have been observed in tissue samples taken after dry needling treatments with needle rotation. Deformation of the extracellular matrix is believed to signal therapeutic effects via the alignment of collagen fibers and fibroblasts. This technique has also been shown to be the only technique that elicits an endogenous opioid release creating true pain reduction from the treatment. If you have any further questions about Dry Needling or feel you could benefit from this treatment technique, please contact Morgan or call our office to speak with one of the therapists at 410-628-0820. Stay tuned for our next newsletter where we will discuss the impact of Dry Needling on the Central Nervous System. References Chu, J. "Does EMG (dry needling) reduce myofascial pain symptoms due to cervical nerve root irritation?." Electromyography and clinical neurophysiology 37.5 (1997): 259-272. Chu, Jennifer. "Twitch-obtaining intramuscular stimulation: observations in the management of radiculopathic chronic low back pain." Journal of Musculoskelatal Pain 7.4 (1999): 131-146. Langevin, Helene M., David L. Churchill, and Marilyn J. Cipolla. "Mechanical signaling through connective tissue: a mechanism for the therapeutic effect of acupuncture." The FASEB Journal 15.12 (2001): 2275-2282. http://www.acupmedvet.com/artigos%20cient%C3%ADficos/Langevin%20et%20al.,%202001b.pdf Langevin, Helene M., David L. Churchill, and Marilyn J. Cipolla. "Mechanical signaling through connective tissue: a mechanism for the therapeutic effect of acupuncture." The FASEB Journal 15.12 (2001): 2275-2282. http://jap.physiology.org/content/91/6/2471.short Langevin, Helene M., et al. "Dynamic fibroblast cytoskeletal response to subcutaneous tissue stretch ex vivo and in vivo." American Journal of Physiology-Cell Physiology 288.3 (2005): C747-C756. http://ajpcell.physiology.org/content/288/3/C747.short Langevin, Helene M., et al. "Subcutaneous tissue fibroblast cytoskeletal remodeling induced by acupuncture: Evidence for a mechanotransduction‐based mechanism." Journal of cellular physiology 207.3 (2006): 767-774. Shah, Jay P., et al. "Biochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger points." Archives of physical medicine and rehabilitation 89.1 (2008): 16-23. http://triggerpoint-tutorial.com/pdf/Shah_Biological_milieu_of_MTP.pdf